Testicular cysts may be caused by cancer, fibrosis or just epidydymal cysts. The symptoms include swelling, lesions, inflammations and problems during ejaculation. Here are all the causes, pictures, removal and other treatments worth knowing.
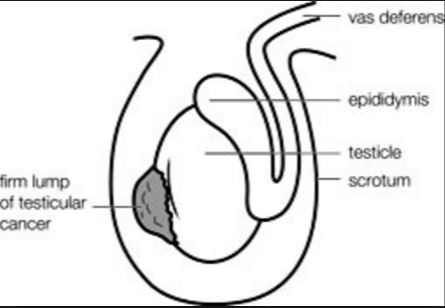
A testicular lump is an abnormal mass in the testicles. The testicles are—the egg-shaped male reproductive glands. They hang below the penis in a sac called the scrotum. Their primary function is to produce sperm and testosterone.
A testicular mass, cyst or lump, may be located in one or both testicles, and is a fairly common condition. Lumps can occur in both men and teenage boys. Testicular lumps are signs of problems with the testicles.
They may be caused by an injury, but they can also indicate a serious underlying medical problem. This article will discuss the causes, symptoms and treatments.
What is a cyst on testicle? Pictures
A cyst on testicles may appear as a small mass, lump or bump. The cyst usually forms on either one or both testicles. Since they are commonly caused by injury or trauma to the testicles, the cysts may be painful. But how do testicular cysts look like? Here are pictures, images and photos to help you identify your symptoms.
Types of testicular masses or lumps
Most testicle lumps occur because of an injury. However, birth defects and other factors can also cause lumps in the testicles. There are different types of masses and cysts on the testicles. They include torsions, hydroceles, varicoceles, cancer masses and epidydymal cysts.
a) Varicocele on testicles
This type of lump is the most common, occurring in about one in every seven men. Enlarged veins in the testicles cause varicocele lumps. They become more noticeable after puberty when blood flow increases in the fully developed testicles.
b) Hydrocele on scrotum sack
A hydrocele testicular lump is caused by the buildup of fluid in the testicles. You are likely to see he sack of testicles having a small bulge. This type of testicular lump occurs in one to two out of every 100 newborn males.
- According to Mayo Clinic. “Older boys and adult men can develop a hydrocele due to inflammation or injury within the scrotum.”
- Hydrocele masses on the scrotum are not painful.
- In most newborns, these cysts will go away on their own without treatment.
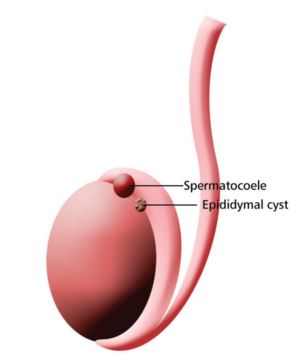
c) Epididymal cyst
An epididymal cyst or spermatocele occurs when the long, coiled tube behind the testicles(epididymis) becomes filled with fluid and cannot drain. If it contains sperm, it is known as a spermatocele. This form of testicular lump affects up to one in three men, and most often resolves on its own.
d) Testicular torsion
Testicular torsion occurs when the testicles become twisted, typically due to an injury or accident. This condition most often occurs in boys between the ages of 13 and 17, but can affect men of all ages. This is a medical emergency and requires urgent investigation and possible treatment.
- Torsion causes complete or partial lack of blood supply to the testicles.
- The most prominent and immediate symptom of torsion is sudden pain.
- Formation of a mass or tumor is also common with these kinds of cysts.
e) Testicular cancer lumps
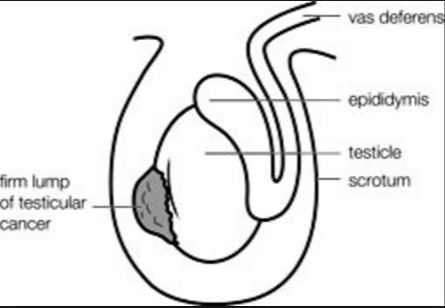
Some testicular cysts and lumps indicate the growth of testicular cancer. Only a doctor will be able to determine if a lump is cancerous. Testicular cancer is the most common type of cancer for American men between the ages of 15 and 34, according to the Mayo Clinic.
Testicular Cysts Causes
Not all lumps indicate the presence of testicular cancer. Nevertheless, a medical professional should examine any changes in the testicles, especially lumps or swelling.
Men over the age of 14 should do monthly testicle self-examination to help spot any lumps early so that they can be properly examined and treated. Here are the causes of cysts on testicles and scrotum.
1. Testicular Cancer
The testicular cysts can also be a sign of cancer. Men with testicular cancer may experience a variety of symptoms or signs. Sometimes, men with testicular cancer do not show any of these symptoms. In addition, these symptoms can be caused by other conditions besides cancer, so the presence of these symptoms does not mean that a man has cancer.
Usually, the first sign of testicular cancer is enlargement of the testicle or a small lump or area of hardness on the testicle sack. Any lump, enlargement, hardness, pain, or tenderness of the testicle should be evaluated by a doctor as soon as possible.
Other symptoms of testicular cancer usually do not appear until after the cancer has spread to other parts of the body. Symptoms of testicular cancer may include:
- Painless lump or swelling on either testicle. If detected early, a testicular tumor may be about the size of a pea or a marble, but it can grow much larger.
- Pain or discomfort, with or without swelling, in a testicle or the scrotum.
- Change in the way a testicle feels or a feeling of heaviness in the scrotum. For example, one testicle may become more firm than the other testicle. Or, testicular cancer may cause the testicle to grow bigger or to become smaller.
- Dull ache in the lower abdomen or groin
- Sudden buildup of fluid in the scrotum
- Breast tenderness or growth. Although rare, some testicular tumors produce hormones that cause breast tenderness or growth of breast tissue, a condition called gynecomastia.
- Lower back pain, shortness of breath, chest pain, and bloody sputum or phlegm can be symptoms of later-stage testicular cancer.
2. Spermatocele cyst on testicles
A spermatocele is an abnormal sac (cyst) that develops in the epididymis — the small, coiled tube located on the upper testicle that collects and transports sperm. Noncancerous and generally painless, spermatocele testicular cysts usually are filled with milky or clear fluid that might contain sperm.
The exact cause of spermatoceles is unknown but might be due to a blockage in one of the tubes that transports sperm. Spermatocele cysts, sometimes called spermatic cysts, are common. They typically don’t reduce fertility or require treatment.
While diagnosing the ultrasound, your doctor will most likely use ultrasound. An ultrasound orsonogram scan is a procedure of using high-frequency sound waves to retrieve the image of a body part.
3. Epydidymal cysts
Another cause of cysts on scrotum or crotch is an epydidymal cyst. A cyst is a sac that is filled with a fluid or semi-fluid material. Cysts develop in various places in the body and arise from different parts (tissues) of the body.
An epididymal cyst is a non-cancerous (benign) growth filled with clear liquid which is found at the top end of the testis (testicle) where the spermatic cord (vas deferens) is attached. This area is known as the epididymis.
This is the inflammation of the epididymis, the comma-shaped structure above and behind the testicle that stores and transports sperm. Epididymitis is often caused by a bacterial infection, including sexually transmitted bacterial infections, such as chlamydia. Less commonly, epididymitis is caused by a viral infection or abnormal flow of urine into the epididymis.
4. Orchitis or viral infections
This is inflammation of the testicle usually due to a viral infection — most commonly mumps. When orchitis is caused by a bacterial infection, the epididymis also might be infected.
5. Hydrocele or painless cyst on scrotum
Hydrocele occurs when there is excess fluid between the layers of a sac that surrounds each testicle. A small amount of fluid in this space is normal, but the excess fluid of a hydrocele usually results in a painless swelling of the scrotum.
In infants, a hydrocele occurs usually because an opening between the abdomen and the scrotum hasn’t properly sealed during development. In adults, a hydrocele occurs usually because of an imbalance in the production or absorption of fluid, often as a result of injury or infection in the scrotum.
6. Hematocele blood cyst on balls
Hematocele occurs where there is blood between the layers of a sac that surrounds each testicle. Traumatic injury, such as a direct blow to the testicles, is the most likely cause of a blood blister on balls.
7. Varicocele
This is the enlargement of the veins within the scrotum that carry oxygen-depleted blood from each testicle and epididymis. Varicocele is more common on the left side of the scrotum because of differences in how blood circulates from each side. A varicocele cyst on testicles might cause infertility
8. Inguinal hernia
This is a condition in which a portion of the small intestine pushes through an opening or weak spot in the tissue separating the abdomen and groin. In infants, an inguinal hernia usually occurs because the passageway from the abdomen to the scrotum has failed to close during development.
An inguinal hernia might appear as a mass in the scrotum or higher in the groin.
9. Testicular torsion
This is a twisting of the spermatic cord, the bundle of blood vessels, nerves and the tube that carries semen from the testicle to the penis.
This painful condition cuts off blood to the testicle and can result in the loss of the testicle if not promptly treated. The affected testicle might be sideways, enlarged and higher than normal.
Symptoms of Testicular Cysts
Symptoms of a testicular lump or cyst on scrotum vary depending on the underlying cause. However, nearly all lumps cause noticeable swelling and changes in the texture of the testicles.
A varicocele rarely causes symptoms. If it does, the affected testicle may feel heavier than the other, or the lump may feel like a small sac of worms.
Painless lumps
A hydrocele is painless in infants, but older boys or men may feel abdominal pressure. It causes visible swelling of the testicles.
Epididymal cysts are also generally painless; one testicle can feel heavier than normal in some men.
Testicular cyst pain
A common symptom is a painful cyst on testicles when raptured or popped. Inflammatory swellings may require anti-inflammatory drugs or painkillers to relieve the discomfort. However, if the pain from the cyst is persistent, see a doctor for proper diagnosis and treatment.
Because it is typically caused by a scrotal injury, testicular torsion can be extremely painful. It is a medical emergency that causes the following symptoms:
- Abdominal pain
- Fever
- Frequent urination
- Nausea
- Swelling of the scrotum
- Vomiting
- A testicle that’s higher than normal or oddly angled
- An unusual lump
- A dull aching pain or feeling of heaviness in the scrotum
- Pain that radiates throughout the groin, abdomen or lower back
- Tender, swollen or hardened testicle
- Tender, swollen or hardened epididymis (ep-ih-did-uh-mis), the soft, comma-shaped tube above and behind the testicle that stores and transports sperm
- Swelling in the scrotum
- Redness of the skin of the scrotum
- Nausea or vomiting
A lump caused by testicular cancer can produce the following symptoms:
- Dull ache in the abdomen or groin
- Swelling or tenderness in the breasts
- Heaviness in the scrotum
- Pain
- Sudden collection of fluid in the scrotum
If the cause of a scrotal mass is an infection, signs and symptoms also might include:
- Fever
- Urinary frequency
- Pus or blood in the urine
Treatment for Testicular Cysts
Pain from a varicocele usually subsides without treatment. However, your doctor may prescribe pain medication or advise that you use over-the-counter pain relievers.
In cases of recurring episodes of discomfort, surgery may be required to eliminate the congestion in the veins.
1. Surgery for Scrotal cyst removal or testicular cyst removal
The surgery may involve either tying off the affected veins or diverting blood flow to those veins through other methods. This causes blood to bypass those veins, which eliminates the swelling.
Treatment for a hydrocele lump may also involve surgery, but it most often clears up on its own by age two. The surgery involves making a small incision in the scrotum to drain excess fluid if natural treatment is not the case.
Hydrocele repair, excision of an epididymal cyst (pictured) and open surgery, laparoscopic surgery or radiological embolisation may be needed for significant symptoms from the swelling. Otherwise, no treatment is necessary.
2. Excision of big cysts on scrotum
An epididymal cyst does not require treatment unless it causes pain or discomfort.
- If the cyst is small and causing no problems you may need no treatment. You just need to keep an eye on it and seek medical advice if it gets larger or becomes painful.
- Children do not usually need treatment because most cysts disappear by themselves. However, surgical removal may be necessary if they become painful or don’t start to shrink.
- Large or painful cysts can be removed surgically. The operation is a simple one and recovery is usually uneventful. Occasionally, infection can set in or you can develop a blood clot in the scrotum (a scrotal haematoma).
3. Sclerotherapy
Sclerotherapy used to be performed as an alternative to surgery. It involves injecting the cyst with a liquid called a sclerosant. However, it is not often done these days as the cyst frequently grows back.
The procedure involves surgically removing the cyst and sealing the scrotum with dissolvable stitches that typically disappear within 10 days.
4. Antibiotics for bacterial infections
Additionally, antibiotics are used for infection of the epididymis. Your GP may refer you to a urologist (if you are over 50 or have a urinary infection) or to a genitomedical clinic (if you are young or your infection may be sexually-acquired).
Testicular involvement with mumps usually requires no specific treatment apart from painkillers. Suspected torsion of the testis requires emergency admission and immediate surgery.
Testicular torsion requires immediate surgery to restore blood flow to the testicle, preventing tissue death.
5. Chemotherapy and radiation
Testicular cancer is treated in the same way as other types of cancer: through surgery, chemotherapy, radiation, and other methods. Treatment method depends on how early the cancer is detected.
Surgical removal of the testicle may be an option to prevent the cancer from spreading to other parts of the body.
A specialist in cancer treatment (oncologist) will recommend treatments based on whether the cancer is isolated to a testicle or has spread to other tissues in the body. Your age and overall health also are factors in choosing treatment options for testicular cancer.
- Radical inguinal orchiectomy. This is the primary treatment for testicular cancer. It’s a surgical procedure to remove the affected testicle and spermatic cord through an incision in the groin. Lymph nodes in your abdomen also might be removed if the cancer has spread to them.
- Radiation therapy. This type of therapy uses high-dose X-rays or other high-energy radiation to kill cancer cells that may remain after removal of the affected testicle.
- This is a drug treatment that uses powerful chemicals to kill cancer cells.
Home Remedies and Care
- Enjoy tomatoes. They contain nutrients that help prevent the formation of cysts.
- Roast up some pumpkin seeds and eat them while still warm.
- Eat foods high in zinc to promote healing.
- Limit foods that are hard on the body such as refined sugars and caffeine.
- Leave the cyst alone unless it causes pain. In most cases they will go away on their own over time.
Sources and References
- Mayo Clinic: Scrotal Masses, Causes, Symptoms and Treatment.
- Hydroceles
- Healthline: Testicle Lump: Causes, Types, Symptoms and Treatments.
- Net: Testicular Cancer Signs and Symptoms.
- British Association of Urological Surgeons: Lumps on Scrotum and Testicles