Testicular torsion, a condition that can evoke fear and anxiety in any man, is often misunderstood. With the potential to cause severe pain and even fertility issues, it’s essential to be well-informed about this condition, also known as twisting of the testicle. This comprehensive guide will delve into the intricacies of testicular torsion, from understanding its causes and symptoms to exploring treatment options and long-term implications. By the end of this article, readers will have a more profound understanding of this condition and the importance of early intervention.
Short Summary
- Testicular torsion is a medical condition that can cause long-term damage or loss of the testicle if left untreated.
- Early detection and treatment with orchiopexy surgery are critical to reduce the risk of complications and preserve fertility.
- Testicular torsion can lead to emotional, psychological, and physical issues which should be addressed through appropriate support services.
Understanding Testicular Torsion
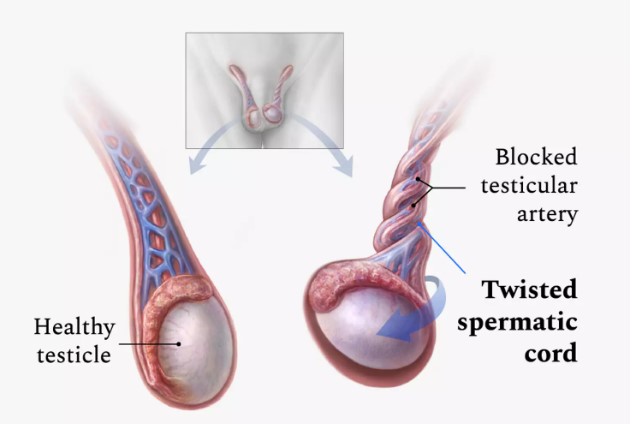
Testicular torsion is a condition in which the spermatic cord, responsible for supplying blood to the testicle, becomes twisted, obstructing blood flow and potentially causing testicular ischemia. This condition requires prompt medical attention, as the longer it remains untreated, the higher the risk of permanent damage or even testicular loss.
So, testicular torsion occurs when certain factors contribute to its development. How does this happen, and what are these factors?
Definition and Occurrence
The spermatic cord carries blood to the testicle. When this cord twists, it interrupts the blood supply causing testicular torsion. This causes sudden and severe pain, swelling, and redness in the affected area. Testicular torsion affects approximately one in 4,000 males under 25 years of age. Importantly, prompt diagnosis and treatment are vital to preventing long-term complications.
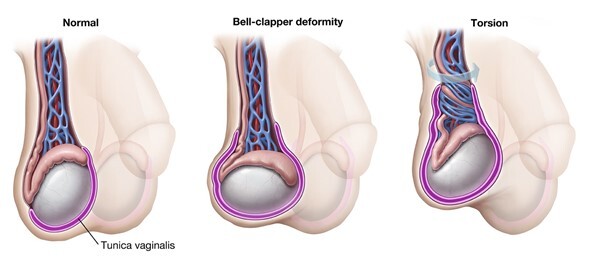
The exact cause of testicular torsion remains uncertain, but certain factors such as the bell clapper deformity, a condition where the testicles hang freely in the scrotum, can predispose someone to this condition. Twisting of the spermatic cord can result from something as simple as a minor injury or even occur spontaneously.
Bell Clapper Deformity
Bell clapper deformity may contribute to the development of testicular torsion, as the testicles can swing freely within the scrotum, akin to a clapper in a bell. This abnormality increases the likelihood of the spermatic cord twisting, which can lead to testicular torsion.
Although not every case of testicular torsion is linked to bell clapper deformity, understanding this risk factor can help raise awareness and emphasize the importance of seeking prompt medical attention if symptoms of testicular torsion are experienced.
Identifying Symptoms of Testicular Torsion

Recognizing testicular torsion symptoms is crucial for early diagnosis and successful treatment. The most common symptoms of testicular torsion are:
- Sudden, severe pain in the scrotum
- Swelling
- Redness
- Tenderness of the affected area
If these symptoms manifest, it is imperative to seek medical attention immediately, as testicular torsion is considered a medical emergency.
So, what specific symptoms should you be on the lookout for?
Acute Scrotal Pain
Acute scrotal pain is characterized by sudden, intense pain in the scrotum, often accompanied by swelling, redness, and tenderness in the affected area. This pain can occur at any time, but is most commonly experienced in the middle of the night or early in the morning. Testicular torsion is a leading cause of acute scrotal pain, and other potential causes include trauma, infection, and inflammation.
It is essential to consult a healthcare provider immediately if you experience sudden pain in the testicle, even if the pain dissipates without treatment. This could be indicative of a medical emergency, and early intervention is crucial to prevent potentially irreversible damage to the testicle.
Swelling and Discoloration
In addition to acute scrotal pain, testicular torsion can cause swelling and discoloration of the affected testicle. As the blood supply to the testicle is obstructed, the testicle may become swollen and discolored. These symptoms should not be ignored, as they could indicate a medical emergency requiring immediate attention.
Surgical intervention is typically recommended to untwist the spermatic cord and restore blood flow to the affected testicle in cases of testicular torsion associated with swelling and discoloration. Prompt treatment is crucial to prevent long-term complications, such as testicular damage and fertility issues.
Diagnosing Testicular Torsion

Once the symptoms of testicular torsion have been identified, the next step is to get testicular torsion diagnosed through a series of tests. The diagnostic process typically includes a physical examination, imaging tests, and a review of the patient’s medical history.
Let’s delve into the specifics of each diagnostic step and understand their role in identifying testicular torsion.
Physical Examination
During the physical examination, the doctor will:
- Inspect the scrotum and testicles for signs of swelling, tenderness, and discoloration
- Assess the cremasteric reflex, which is the involuntary contraction of the testicle when the inner thigh is stroked
- Inspect for a mass or an enlarged epididymis
- Check for a hydrocele or a hernia
The physical examination plays a vital role in diagnosing testicular torsion and helps the doctor determine the appropriate course of action. In some cases, further testing may be needed to confirm the diagnosis.
Imaging Tests
Imaging tests, such as a scrotal ultrasound, can assist in diagnosing testicular torsion. The ultrasound can reveal whether the testicle is twisted or not, providing vital information to guide treatment decisions. In some cases, other imaging tests like MRI or even urine tests may be employed to aid in the diagnosis.
The combination of physical examination and imaging tests helps healthcare professionals accurately diagnose testicular torsion and determine the most effective treatment plan. Early diagnosis is essential to prevent long-term complications and ensure the best possible outcome for the patient.
Treatment Options for Testicular Torsion
Upon diagnosing testicular torsion, including neonatal testicular torsion, it is important to know that it requires surgery. The primary treatment option is testicular torsion surgery, specifically a procedure called orchiopexy. This involves untwisting the spermatic cord and securing the testicle to the inner lining of the scrotum to prevent future occurrences of torsion, such as testicle twists. Time is of the essence in these cases, as the longer the torsion remains untreated, the higher the risk of irreversible damage to the testicle. With prompt intervention, testicular torsion treated effectively can minimize complications and preserve testicular function.
What does the treatment process entail, and what can patients expect during recovery?
Surgical Intervention
During the orchiopexy procedure, the surgeon will:
- Make a small incision in the scrotum
- Untwist the spermatic cord
- Secure the testicle to the inner lining of the scrotum to prevent future occurrences of torsion
This surgical intervention is typically performed as an emergency procedure to minimize the risk of permanent damage to the testicle. In some cases, if the torsion has caused severe damage to the testicle, it may need to be surgically removed.
The surgery is typically performed under general anesthesia, and the recovery process involves monitoring for infection, taking prescribed pain medications, and refraining from strenuous activities for a few weeks. Prompt surgical intervention is crucial for the patient’s long-term wellbeing and fertility.
Post-Surgery Care
After the surgery, patients can expect some discomfort in the initial few days, with swelling or bruising on the scrotum or groin lasting approximately one week. As the pain subsides, patients can gradually resume their usual activities, including work or school. It is recommended to steer clear of any strenuous or heavy activities like sports, for a minimum of 3 to 4 weeks. This includes activities such as heavy lifting.
Follow-up appointments are crucial in the recovery process, as they allow the doctor to monitor healing progress and address any potential complications. Patients should contact their healthcare provider if they experience any symptoms after surgery, as prompt intervention can help minimize the risk of complications and ensure a smooth recovery.
Preventing Testicular Torsion Recurrence
Surgery is the only method to prevent future occurrences of testicular torsion. The surgical procedure, called orchiopexy, involves securing the testicle to the inner lining of the scrotum, reducing the risk of the testicle twisting in the future. Early intervention is critical to prevent irreversible damage to the testicles and ensure the best possible outcome.
How can orchiopexy be used to prevent testicular torsion, and why is early detection so crucial?
Orchiopexy for Prevention
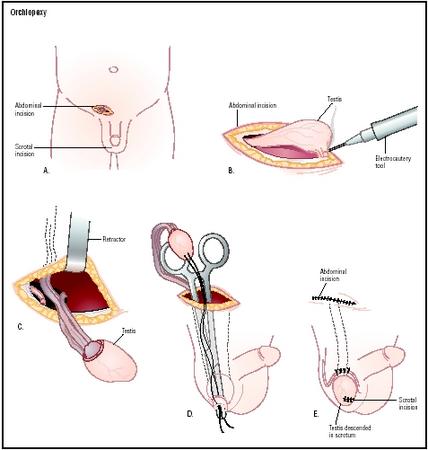
Orchiopexy is a procedure in which the testicle is relocated from the groin to the scrotum, effectively securing it in place and reducing the risk of torsion. This procedure can be performed to prevent testicular torsion in the unaffected testicle, providing additional security and peace of mind for the patient.
While orchiopexy carries some risks, such as infection, bleeding, and damage to the testicle or surrounding tissue, the benefits of preventing future occurrences of testicular torsion and preserving the patient’s fertility far outweigh the potential risks.
Importance of Early Detection
The significance of early detection of testicular torsion cannot be overstated. Prompt diagnosis and treatment can help prevent complications such as testicular infarction, necrosis, and sub/infertility. Delayed detection and treatment may lead to permanent damage to the testicle, necessitating surgical removal and potentially impacting the patient’s fertility.
Being aware of the symptoms and risk factors of testicular torsion, as well as the importance of early intervention, can help individuals take prompt action in the event of a torsion, minimizing the risk of long-term complications and preserving fertility.
Complications and Long-Term Effects of Testicular Torsion

Testicular torsion can have a lasting impact on an individual’s physical and emotional wellbeing. The complications and long-term effects of this condition can range from fertility issues to emotional and psychological distress.
Understanding these implications is crucial for patients and their families, as it helps them navigate the challenges associated with testicular torsion and seek appropriate support when needed.
Testicular Damage and Fertility
Testicular torsion may result in permanent damage to the testicle, which can lead to fertility issues. The extent of the damage depends on the duration of the torsion and the effectiveness of the treatment. In cases where the torsion is not addressed within six hours, the testicle may suffer irreversible damage, necessitating surgical removal.
The loss of a testicle can be emotionally challenging for some individuals, as it may lead to feelings of loss, grief, and insecurity. In such cases, a prosthetic testicle may be considered to help restore the patient’s self-esteem and confidence.
Emotional and Psychological Effects
In addition to the physical complications, testicular torsion can also have a profound emotional and psychological impact on individuals. Heightened levels of anxiety, fear of recurrence, and potential psychiatric or behavioral issues can result from this condition.
Feelings of guilt, shame, and embarrassment may also arise, which can adversely affect one’s self-esteem and relationships. Seeking emotional support from friends, family, or a mental health professional can be instrumental in helping individuals cope with the emotional and psychological effects of testicular torsion.
Summary
Testicular torsion is a medical condition that requires prompt attention and intervention to prevent long-term complications and preserve fertility. Understanding the causes, symptoms, diagnostic process, and treatment options is crucial for individuals at risk of this condition. By being well-informed and proactive, individuals can significantly reduce the risk of complications and ensure the best possible outcome for their physical and emotional wellbeing.
Frequently Asked Questions
- How do you fix a twisted testicle?
- Testicular torsion requires surgical intervention to untwist the spermatic cord and restore normal blood flow. If the testicle is healthy, the surgeon will then stitch it in place to prevent future twisting.
- Surgery is usually done under general anesthesia, and the other testicle is also stitched to prevent torsion from occurring again.
- What happens if a testicle gets twisted?
- Testicular torsion is a medical emergency that cuts off the blood supply and causes sudden pain and swelling. If left untreated, it can lead to a damaged or dead testicle which must then be removed.
- It requires immediate medical attention and surgery to save the testicle.
- How long can a testicle stay twisted?
- Testicular torsion is an emergency and requires timely medical attention. Generally, the testicle can be saved 90% of the time if treatment is received within 4-6 hours of the start of torsion; this rate drops to 50% after 12 hours and 10% after 24 hours.
- How do you know if you have testicular torsion?
- If you experience sudden, severe pain in the scrotum along with swelling, redness or hardening of the scrotum, and one side becoming larger than the other, you should seek medical advice as this could be a sign of testicular torsion.
- What is the primary cause of testicular torsion?
- Testicular torsion is thought to be caused by a predisposing factor such as the bell clapper deformity.