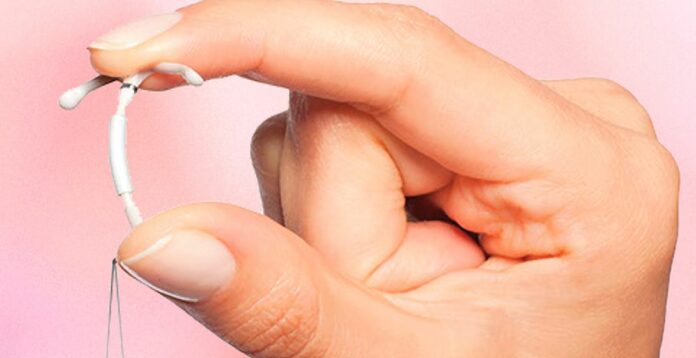
IUDs, or intrauterine devices, have a long and fascinating history. These small, T-shaped contraceptives have been around for decades and are known for their effectiveness in preventing pregnancy.
We’ll discuss the different types of IUDs available today and examine their pros and cons. We’ll address common misconceptions about IUDs and provide valuable insights into their usage, woman, endometrial lining, womb. Whether you’re considering an IUD for contraception or simply want to broaden your knowledge on reproductive health options, this post will equip you with essential information to make informed decisions regarding your sexual health.
Key Takeaways
- IUDs are a long-term, reversible birth control method that can be inserted and removed by a healthcare professional.
- Understanding the benefits and risks of using IUDs is crucial for making an informed decision about birth control options.
- The procedure for inserting an IUD is relatively quick and can be done during a routine office visit.
- It’s important to consider the cost, duration, and potential side effects of IUDs before making a decision.
- After IUD insertion, individuals may experience mild discomfort, but recovery is generally quick.
- IUD removal is a simple procedure that can be done by a healthcare provider when the individual decides to discontinue using the IUD.
Understanding IUDs
Hormonal
Hormonal IUDs release progestin, a hormone that prevents ovulation. This means that the ovary does not release an egg each month.
These devices also thicken cervical mucus, making it difficult for sperm to reach the egg. As a result, fertilization becomes less likely.
Hormonal IUDs can reduce menstrual bleeding and cramping. They are effective for 3 to 6 years, depending on the specific type.
Common brands include Mirena, Kyleena, and Liletta. These are well-known names in the realm of hormonal intrauterine devices.
Some women prefer hormonal IUDs, as they often lead to lighter periods or even no periods at all while providing highly effective birth control.
Hormonal intrauterine devices have gained popularity due to their convenience and effectiveness in preventing pregnancy without requiring daily action from users.
Copper
Copper IUDs use copper to create an environment hostile to sperm within the uterus. The presence of copper makes it difficult for sperm to survive and move towards the egg.
Unlike hormonal options, copper IUDs do not contain any hormones themselves. This makes them suitable for those who cannot use hormonal contraceptives due to medical reasons or personal preferences.
Copper IUDs can remain effective for up to 10 years after insertion into the uterus.
Examples of copper IUD brands include Paragard and other T-shaped devices designed specifically with this non-hormonal approach in mind.
The absence of hormones is appealing for many individuals seeking long-term contraception without affecting their natural hormone levels.
Longevity
Both types of intrauterine devices offer long-term protection against pregnancy when properly inserted by a healthcare professional.
Hormonal IUDs can last anywhere from 3-6 years before needing replacement, depending on which brand is chosen by the individual based on consultation with their doctor or healthcare provider. On the other hand, copper-based options provide protection against unwanted pregnancies for up to a decade after insertion into the uterus.
How IUDs Work

Preventing Fertilization
IUDs meaning intrauterine devices, prevent fertilization by blocking sperm from reaching the egg. They achieve this by interfering with the ability of sperm to fertilize eggs in various ways. This prevents pregnancy without affecting ovulation or hormone levels. With over 99% effectiveness in preventing pregnancy, IUDs offer immediate contraceptive action upon insertion.
The copper IUD creates an environment that is toxic to sperm, thereby preventing their survival and movement within the uterus. On the other hand, hormonal IUDs release progestin, which inhibits sperm function and survival. Both types of IUDs hinder sperm from successfully fertilizing an egg.
IUDs work by thickening cervical mucus, creating a barrier that makes it difficult for sperm to travel through the cervix and reach the egg. This natural mechanism reduces the likelihood of fertilization and supports the contraceptive effect of IUDs effectively.
Thickening Cervical Mucus
Hormonal IUDs thicken cervical mucus as a means of creating a barrier to prevent fertilization. The thickened mucus hinders sperm mobility and reduces their chances of reaching and fertilizing an egg.
This method offers a non-hormonal approach that aligns with women’s reproductive system’s natural processes while providing highly effective contraception.
Thickened cervical mucus acts as a physical barrier against sperm entry into the uterus, complementing other mechanisms employed by hormonal or copper-based IUD devices.
Inhibiting Sperm
Both hormonal and copper-based IUD methods inhibit the functioning of sperms in unique ways. Hormonal IUD releases progestin which inhibits sperms’ function and survival within the female reproductive system.
Copper-based IUD creates an environment hostile to sperms through its toxic effects on them thus hindering their movement within uterine cavity.
Benefits of Using IUDs
Longevity
IUDs, or intrauterine devices, are a long-term birth control method that offers extended protection against pregnancy. Hormonal IUDs can effectively prevent pregnancy for 3 to 6 years, depending on the brand. For instance, Mirena and Kyleena can last up to 5 years, while Skyla is effective for 3 years. On the other hand, copper IUDs have an even longer lifespan and can provide protection for up to 10 years after insertion. This longevity makes them a convenient option for women who prefer not to worry about their birth control method frequently.
The fact that inert IUDs can remain in place and protect against pregnancy without needing regular replacements like other methods such as pills or patches makes them highly appealing to many women. For example, if a woman chooses hormonal IUD insertion at age 25 and plans on starting a family at age 30, she does not need to think about her contraception during those five years.
Another example could be a woman who has completed her family planning but still wants reliable contraception until menopause; in this case, copper IUD insertion would be an excellent choice due to its extended effectiveness.
Effectiveness
IUDs are incredibly effective at preventing pregnancy when used correctly. In fact, they are more than 99% effective, making them one of the most reliable forms of birth control available today. This level of effectiveness is comparable to permanent sterilization methods like tubal ligation or vasectomy.
Moreover, once inserted by a healthcare professional following proper procedures and guidelines (as discussed in the previous section), minimal user intervention is required with these devices – contributing significantly to their high efficacy. The low maintenance aspect combined with their exceptional effectiveness makes IUD use very attractive compared to other contraceptive options.
For instance: A young couple may choose an inert hormonal IUD over permanent sterilization options because it allows flexibility for future family planning decisions without compromising reliability during the chosen period. Another scenario might involve someone seeking long-term contraception but wanting something reversible; they could opt for an inert copper IUD instead of permanent solutions due to its comparable effectiveness.
Convenience
One significant advantage of using an intrauterine device is its convenience once inserted into the uterus by a healthcare provider – there’s no daily or monthly maintenance required afterward. This means that women do not have any interruptions in their contraceptive coverage due to missed doses or appointments as seen with some other birth control methods such as pills or patches.
Additionally: Women who lead busy lives may find this type of long-lasting contraception particularly convenient since it doesn’t require frequent attention post-insertion. Furthermore: The immediate resumption of normal activities after insertion also adds another layer of convenience since there’s no waiting period before achieving full contraceptive protection.
Procedure for Inserting an IUD
Preparation
Before the iud insertion, the healthcare provider will discuss your medical history, conduct a pelvic exam, and possibly perform tests for sexually transmitted infections. They may also recommend taking pain medication prior to the procedure.
Once you’re ready for the insertion, you’ll be asked to lie on an examination table with your feet placed in stirrups. The healthcare provider will then proceed with cleaning your cervix and vagina before using a speculum to gently hold open the vaginal walls.
Insertion Steps
During iud insertion, the healthcare provider will measure your uterus and then carefully insert the IUD through the cervix into your uterus. This process is relatively quick and typically causes only mild discomfort or cramping.
After ensuring that the IUD is correctly positioned inside your uterus, they will trim any excess strings protruding from it. Once everything is in place, they’ll remove the speculum and allow you some time to rest before leaving.
Post-insertion Care includes being vigilant about any unusual symptoms such as severe pain or heavy bleeding after getting an IUD inserted. It’s important to attend all scheduled follow-up appointments as well.
Cost and Duration of IUDs
Expense Factors
The cost of an IUD can vary based on several factors. One significant factor is the type of IUD chosen, as there are hormonal and copper options available. The hormonal IUD tends to be slightly more expensive than the copper one due to the additional cost of hormones. Another important expense factor is whether or not a healthcare provider covers the insertion procedure in their fee. Some clinics may charge separately for the device itself and its insertion, while others may offer an all-inclusive package.
Moreover, consider that there might be additional expenses, such as consultation fees with healthcare providers prior to getting an IUD inserted. These consultations are essential for determining if an individual is a suitable candidate for this form of birth control. It’s also crucial to take into account any potential follow-up appointments that may incur extra costs.
Lastly, it’s worth noting that certain organizations or government programs might provide financial assistance or subsidies for individuals seeking contraceptive methods like IUDs.
Insurance Coverage
Many insurance plans typically include this form of contraception under their benefits package. However, it’s vital to verify coverage details with the insurance provider beforehand because policies can differ widely regarding what they cover and how much they reimburse.
Some insurance plans may fully cover both the cost of the device itself and its insertion procedure without requiring any out-of-pocket payment from policyholders. On the other hand, some plans could necessitate a copayment or coinsurance amount from individuals receiving an IUD.
It’s also important to note that those without insurance coverage should explore alternative avenues such as family planning clinics which often offer sliding-scale fees based on income level.
Effective Period
The effective period refers to how long an IUD remains functional once inserted within a woman’s uterus before needing replacement or removal. This duration varies depending on whether one has opted for a hormonal or copper-based device: Hormonal IUDs typically last between 3-6 years whereas copper ones have a lifespan ranging from 10-12 years.
One benefit associated with longer-lasting devices like copper-based ones is reduced overall expenditure compared to shorter-term solutions since fewer replacements are required over time.
Furthermore, understanding this effective period plays into financial considerations when deciding on birth control methods since longer-lasting options can potentially lead to lower cumulative costs over time.
Side Effects and Risks of IUDs
Common Side Effects
IUDs, or intrauterine devices, are a popular form of long-acting reversible contraception. While they are highly effective in preventing pregnancy, copper IUDs can come with some common side effects. Many women experience heavier periods and increased cramping after the insertion of a copper IUD. This is because the device can cause irritation inside the uterus, leading to these symptoms. It’s important to note that while these side effects can be uncomfortable, they often decrease over time as the body adjusts to the presence of the IUD.
Another common side effect associated with copper IUDs is spotting between periods. Some women may notice light bleeding outside their regular menstrual cycle for several months after getting an IUD inserted. However, this typically diminishes over time as well.
In addition to these common side effects, some women using copper IUDs might also experience backaches and discomfort during sexual intercourse. These issues usually occur shortly after insertion but tend to subside as your body gets used to having an IUD.
Severe Risks
While most users tolerate copper IUDs well without experiencing any severe risks or complications, there are rare cases where serious problems can arise. One potential risk is a condition called pelvic inflammatory disease (PID). Although it’s uncommon, PID occurs when bacteria enter the uterus during or after insertion of an intrauterine device. Infections like PID need prompt medical attention and treatment with antibiotics; otherwise, they could lead to long-term health consequences such as infertility or chronic pelvic pain.
Ectopic pregnancy is another severe risk associated with copper IUD use. If a woman becomes pregnant despite having an implanted device in place, there’s a higher chance that her pregnancy will develop outside the womb (ectopic pregnancy), which poses significant health risks and requires immediate medical intervention.
Furthermore, although extremely rare, perforation of the uterus during insertion presents another critical risk linked to copper IUD use. This happens when part or all of the device punctures through the uterine wall into surrounding organs such as the bladder or intestines.
Suitability Concerns
Before deciding on getting a copper IUD placed for birth control purposes, certain suitability concerns need consideration by individuals seeking this contraceptive method. Women who have had previous ectopic pregnancies should carefully weigh their options before choosing a copper IUID due to its association with increased risk for future ectopic pregnancies. Additionally , individuals allergic to copper should avoid using Copper T380A since it contains traces of this metal.
Pain and Recovery after IUD Insertion
Insertion Discomfort
Some women may experience discomfort or pain. This is due to the process of inserting a small device through the cervix into the uterus. The sensation can vary from person to person, with some feeling only mild cramping while others might experience more intense pain.
The discomfort during insertion typically lasts for a short period, usually no longer than a few minutes. Healthcare providers often recommend taking over-the-counter pain relievers before the procedure to help manage any potential discomfort. Deep breathing exercises or using relaxation techniques during insertion can also alleviate some of the temporary discomfort associated with this process.
For those concerned about experiencing significant pain during insertion, discussing these worries with their healthcare provider beforehand can be helpful. Providers may offer additional guidance or options for managing potential discomfort during the procedure.
Recovery Timeline
After IUD insertion, individuals may experience cramping and spotting for several days following the procedure. It’s important to note that recovery experiences vary among different people; therefore, it’s essential not to compare one’s recovery timeline directly with others’.
In general, most individuals find that their symptoms improve within a few days post-insertion as their bodies adjust to the presence of the IUD. However, it’s normal for some individuals to continue experiencing intermittent cramping or light bleeding in the weeks following insertion.
Understanding that every person’s body reacts differently is crucial when considering recovery timelines after IUD placement. While some individuals might feel fully recovered within a week, others may take longer before noticing a reduction in symptoms such as cramping and spotting.
Managing Pain
When looking at ways of managing pain after an IUD insertion, there are several strategies that can help ease any discomfort experienced during recovery. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are commonly recommended by healthcare providers to alleviate cramping and reduce inflammation post-insertion.
Applying heat packs or hot water bottles on your lower abdomen where you’re experiencing cramps can also provide relief from discomfort caused by uterine contractions triggered by the presence of an inserted IUD. Staying hydrated and getting adequate rest are essential components in aiding recovery from any associated pain following an IUD placement procedure.
It’s important for individuals who have recently had an IUD inserted not only seek medical advice if they encounter severe or prolonged pain but also remember that mild-to-moderate levels of discomfort are common initially and should gradually subside as their bodies adapt.
IUD Removal Process
When to Remove
An IUD removal may be necessary for various reasons, such as the end of its lifespan, desire to conceive, or experiencing discomfort. The typical duration for a hormonal IUD is around three to six years, while copper IUDs can last up to 12 years. If you’re considering pregnancy or if your IUD has reached its expiration date, it’s time to think about having it removed.
When thinking about IUD removal, consider consulting your healthcare provider before making any decisions. They can assess the condition of the device and provide guidance on when it should be removed based on your specific situation. Keep track of your device’s expiration date and discuss any concerns with your healthcare provider promptly.
It’s crucial not to attempt removing an IUD by yourself; always seek professional medical assistance from a qualified healthcare provider who can safely remove the device using proper techniques and equipment.
Removal Steps
The process of removing an IUD involves several steps that are typically carried out during a routine visit to a healthcare provider’s office. Firstly, you’ll lie down on an examination table similar to when the device was inserted initially. Your healthcare provider will then use a speculum to gently open the vagina and locate the strings attached at the base of the cervix.
Next, they will carefully grasp these strings with forceps and slowly pull them until they can reach and remove the entire device from within your uterus. You might experience mild cramping or discomfort during this process but remember that this is usually brief and manageable for most individuals.
Afterwards, following confirmation that both arms of the T-shaped frame have been collapsed inward (for hormonal IUDs), ensuring safe removal without causing damage or pain upon extraction from inside your uterus is essential.
Lastly, after successful extraction,your doctor may advise you on post-removal care, which includes monitoring for any unusual symptoms like heavy bleeding or severe pain in case there are complications post-removal.
Post-Removal Care
Once you’ve had your IUD removed, paying attention to how your body responds afterward is crucial. It’s normal to experience some spotting or light bleeding immediately after removal but consult with your healthcare provider if this persists excessively beyond a few days.
You may also notice changes in menstrual patterns following removal; some individuals report heavier periods initially while others find their periods become lighter over time as their body readjusts hormonally.
In addition,if you were using an hormonal-based IUD, remember that fertility typically returns rapidly after its removal compared with other contraceptive methods due do its localized effect within reproductive organs rather than systemic impact throughout entire body.
IUDs After Childbirth and During Menstruation
After giving birth, many women consider different birth control options. One of the choices available is using an intrauterine device (IUD). The IUD can be inserted immediately after childbirth or during a postpartum visit. This timing is convenient for new mothers who may want to avoid getting pregnant again soon after giving birth.
Postpartum insertion of an IUD has several advantages. Firstly, it provides long-term protection against pregnancy without requiring daily attention like other forms of contraception such as pills or condoms. Secondly, it doesn’t interfere with breastfeeding and has no impact on breast milk production.
Furthermore, since the uterus is still enlarged after childbirth, inserting an IUD at this time may be less uncomfortable compared to when the uterus returns to its normal size later on.
Menstrual Impact
The use of IUDs can have varying effects on menstruation for different individuals. Some women experience changes in their menstrual cycle after having an IUD inserted while others notice little difference.
For some women, especially those using hormonal IUDs, periods become lighter and less painful over time. This can be beneficial for those who struggle with heavy bleeding or painful cramps during their period.
On the other hand, some women might experience irregular spotting between periods during the initial months after getting an IUD fitted into their uterus.
Overall, while there’s a possibility that menstrual patterns will change with the use of an intrauterine device, these changes are often manageable and not considered detrimental by many people.
Partner Sensation
One concern that some couples have regarding IUDs is whether they affect sexual experiences due to its placement in the womb near the cervix.
However, research indicates that most partners do not feel any discomfort or sensation during intercourse caused by the presence of an IUD in their partner’s uterus. In fact, once properly positioned inside the uterus by a healthcare provider following insertion, the strings attached to the end of certain types of IUDs usually soften over time and typically don’t cause discomfort for either partner during sex.
Fertility and Health Considerations with IUDs
Resuming Fertility
Many individuals wonder about their fertility after using an IUD. The good news is that fertility usually returns quickly after the removal of an IUD. Unlike some other forms of birth control, such as implants or injections, which might take a while for fertility to return to normal, women who have had an IUD removed can often get pregnant right away. In fact, studies have shown that 87% of women who want to conceive become pregnant within a year of having their IUD removed.
However, it’s essential for individuals considering pregnancy after using an IUD to consult with their healthcare provider. While the majority experience no issues getting pregnant post-IUD removal, there is still a small risk of developing complications such as ectopic pregnancy.
One potential concern related to resuming fertility after using an IUD is the possibility of experiencing ectopic pregnancies. An ectopic pregnancy occurs when a fertilized egg implants itself outside the uterus instead of inside it. This situation can be dangerous and potentially life-threatening if not addressed promptly. Although rare, research has shown that there may be a slightly higher risk for ectopic pregnancies in women who have used certain types of copper-based IUDs compared to those who haven’t used any birth control.
Cancer Influence
The influence on cancer development due to using intrauterine devices (IUDs) has been extensively studied by researchers worldwide. Fortunately, numerous studies have indicated that there is no increased risk of developing cervical or breast cancer associated with using hormonal or copper-based IUDs.
In fact, some research suggests that hormonal IUDs could even offer protective benefits against certain types of cancers such as endometrial cancer – this type originates in the lining cells of the uterus – due to their ability to regulate menstrual bleeding and reduce estrogen exposure over time.
While these findings are reassuring for many individuals considering using an IUD, it’s crucial for anyone concerned about how contraceptives might affect their cancer risks should seek guidance from healthcare professionals before making decisions regarding birth control methods.
Medical Precautions
Before deciding on whether or not they should use intrauterine devices (IUDs), individuals must consider various medical precautions associated with this form of contraception. One important consideration relates specifically to women at higher risk for sexually transmitted infections (STIs). It’s vital for them and all others seeking contraceptive options like IUCDs understand that these devices do not protect against STIs; therefore additional protection through condom usage is necessary when preventing STIs becomes imperative.
Another medical precaution pertains particularly towards people with existing pelvic inflammatory disease (PID). For those suffering from PID – an infection affecting reproductive organs caused by bacteria from untreated STIs – introducing foreign objects into the uterus via intrauterine devices could pose potential risks like worsening inflammation.
Lastly but importantly concerning medical precautions involves carefully discussing one’s health history including any previous gynecological conditions and current medications taken prior receiving insertion approval from healthcare providers.
Historical and Future Perspectives of IUDs
Development History
In the 1920s, Ernst Gräfenberg, a German gynecologist, introduced the concept of intrauterine devices (IUDs) for contraception. These early versions were made of silkworm gut or silver wire and had high rates of complications. However, in the 1960s, Dr. Jack Lippes developed a plastic IUD that significantly reduced these risks. This marked a turning point in the history of IUD development.
The introduction of copper-based IUDs in the 1970s further revolutionized contraceptive options for women worldwide. The copper IUD was found to be highly effective at preventing pregnancy while also being hormone-free. This breakthrough addressed concerns about hormonal side effects associated with other birth control methods.
Despite their long history, modern advancements have continued to enhance IUD technology and effectiveness over time.
Modern Advancements
Advancements in IUD technology have led to improved designs that offer greater safety and efficacy. For instance, contemporary devices are typically T-shaped which helps prevent expulsion from the uterus while providing more reliable contraception.
Moreover, some modern IUD models are equipped with added benefits beyond contraception alone. Hormonal IUDs release progestin into the uterus which not only prevents pregnancy but also reduces menstrual bleeding and cramping for many women.
Another notable advancement is the development of smaller insertion devices which make it easier for healthcare providers to insert an IUD with minimal discomfort for patients.
Future Trends
Looking ahead, future trends in IUD usage suggest increasing popularity due to their convenience and long-term reliability as a reversible form of birth control. As more people seek sustainable family planning methods without daily maintenance or frequent medical visits, long-acting reversible contraceptives (LARCs) like hormonal and copper-based IUDs are expected to gain even more traction.
Furthermore, ongoing research aims to improve existing designs by making them even more user-friendly while enhancing their contraceptive efficacy. One promising area involves exploring new materials that could potentially reduce side effects or increase overall comfort during use.
Final Remarks
You’ve now got the lowdown on IUDs – how they work, their benefits, potential risks, and even the historical and future perspectives. Armed with this knowledge, you can make an informed decision about whether an IUD is right for you. Whether it’s the convenience, long-term effectiveness, or minimal maintenance that appeals to you, remember that your health and well-being are what matter most. If you’re considering an IUD, consult with your healthcare provider to discuss your options and address any concerns you may have. Your body, your choice!
Frequently Asked Questions
What are IUDs and how do they work?
IUDs, or intrauterine devices, are small T-shaped contraceptives placed inside the uterus to prevent pregnancy. They work by altering the uterine environment to deter sperm movement and disrupt fertilization.
Are there any benefits of using IUDs?
Yes, IUDs offer long-term contraception without daily maintenance. They also provide high effectiveness rates and can be easily removed if pregnancy is desired.
What is the procedure for inserting an IUD?
The insertion process involves a healthcare provider placing the IUD into the uterus through the cervix. It’s a relatively quick procedure that can cause mild discomfort but typically doesn’t require anesthesia.
What are some common side effects and risks associated with using IUDs?
Common side effects include cramping, irregular bleeding, and changes in menstrual flow. There’s also a slight risk of pelvic infection during insertion and potential expulsion of the device.
How does fertility come into play when considering an IUD?
After removal, fertility generally returns quickly. Unlike some other forms of birth control, such as hormonal methods that may delay fertility after discontinuation, most women can conceive shortly after removing an IUD.